Services
Chronic Pancreatitis
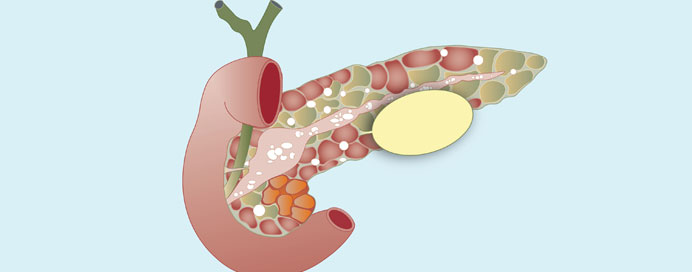
Chronic pancreatitis is a progressive inflammatory condition characterized by long-term inflammation of the pancreas, leading to irreversible damage to the organ. This condition often results from repeated episodes of acute pancreatitis, although other factors such as alcohol abuse, gallstones, autoimmune diseases, or genetic predispositions can also contribute to its development. Chronic pancreatitis typically manifests with persistent abdominal pain, which may worsen after meals or be accompanied by nausea, vomiting, and weight loss. Over time, chronic inflammation can lead to complications such as pancreatic insufficiency, where the pancreas fails to produce enough digestive enzymes or insulin, resulting in malabsorption, steatorrhea, and diabetes mellitus. Diagnosis of chronic pancreatitis involves a combination of medical history, imaging studies (such as CT scans or MRIs), and laboratory tests to assess pancreatic function. Management of chronic pancreatitis focuses on pain management, pancreatic enzyme replacement therapy, dietary modifications, and addressing underlying causes such as alcohol cessation. In advanced cases, surgical interventions may be necessary to relieve pain, remove pancreatic stones, or improve drainage of the pancreatic ducts. Early diagnosis and intervention are crucial in managing chronic pancreatitis and preventing complications, as the condition can significantly impact a patient's quality of life and overall health.